Staphylococcus
Staphylococci are part of the normal flora and important human pathogens. There are more than 26 species but only a few are pathogenic. Staphylococcus aureus is the most invasive species, which can be differentiated from other species by its possession of the enzyme coagulase.Staphylococcus aureus
Asymptomatic carriage of S. aureus is found in up to 40% of healthy people, in the nose, skin, axilla or perineum. This is important in healthcare workers especially if they carry an invasive or resistant strain (e.g. MRSA).
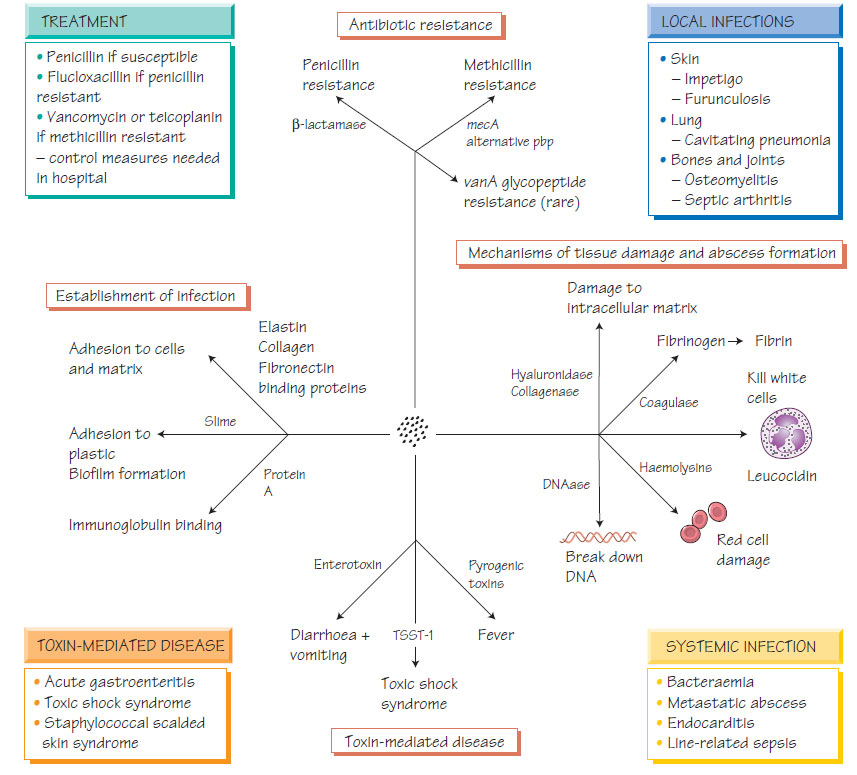
Pathogenesis
Staphylococcus aureus has many potential pathogenicity determinants such as coagulase, which catalyses the conversion of fibrinogen to fibrin thereby providing protection.
| Determinant | Activity | Effect |
| Coagulase | Converts fibrinogen to fibrin | May form protective barrier |
| Adhesion molecules | Bind fibronectin and collagen | Assist adherence |
| Lytic enzymes | Lipase | Breaks down host tissue |
| Protein toxins | Panton–Valentine leucocidin (PVL) toxin | Tissue damage |
| Toxic shock syndrome toxin (TSST) | Shock and toxicity | |
| Enterotoxins | Diarrhoea | |
| Biofilm formation | Slower growth in an extracellular matrix | Difficult to treat with antibiotics, adhere to plastics |
Staphylococcus aureus causes a wide range of infectious syndromes.
- Primary skin infection - impetigo, which is transmitted from person to person.
- Secondary skin infections - associated with eczema, surgical wounds, intravenous devices, burns.
- Pneumonia - rare, but may follow influenza and progress rapidly with cavity formation (see Influenza viruses).
- Endocarditis - can be rapid and destructive; associated with intravenous drug misuse or colonization of intravenous devices (see Endocarditis, myocarditis and pericarditis).
- Osteomyelitis (see Infections of the bones and joints).
- Septic arthritis (see Infections of the bones and joints).
Laboratory diagnosis
Staphylococcus aureus grows readily on most laboratory media. Selective medium contains high salt, to which S. aureus is relatively tolerant. Phenotypic identification depends on demonstrating coagulase, catalase enzymes and typical 'cluster of grapes' morphology on Gram stain. Typing by molecular means can support interventions to control outbreaks.
The history of the susceptibility of S. aureus is a lesson in the history of antimicrobial chemotherapy.
- It was initially susceptible to penicillin, but strains that produced β-lactamase soon predominated, so methicillin and related agents (e.g. flucloxacillin) were introduced and replaced penicillin.
- Methicillin-resistant S. aureus (MRSA) emerged. Resistance is caused by possession of the mecA gene, which codes for a penicillin- binding protein that binds the drug less well. Glycopeptides, such as vancomycin or teicoplanin, started to be required for these strains.
- Intermediate or heteroresistance to glycopeptides emerged as an increasing issue and fully glycopeptide-resistant strains (GRSA) have now been described, resistance being mediated by the vanA vanB genes acquired from enterococci.
Other antibiotics that remain effective include linezolid, aminoglycosides, erythromycin, clindamycin, fusidic acid, chloramphenicol and tetracycline.
In methicillin-sensitive strains, first- and second-generation cephalosporins are effective. Fusidic acid may be given with another agent; it is often given in bone and joint infections (see Infections of the bones and joints) because of its tissue penetration.
Staphylococcus aureus spreads by airborne transmission and via the hands of healthcare workers. Patients colonized or infected with MRSA or GRSA should be isolated in a side room with wound and enteric precautions (see Infection in the hospital environment). Staff may become carriers and disseminate the organism widely in the hospital environment. Carriage may be eradicated by using topical mupirocin and chlorhexidine.
Staphylococcus epidermidis
Staphylococcus epidermidis is the most important of the coagulasenegative staphylococci (CoNS). Once dismissed as contaminants, these organisms are now recognized as pathogens if conditions favour their multiplication.
Staphylococcus epidermidis causes infection of intravenous cannulae, long-standing intravascular prosthetic devices, ventriculoperitoneal shunts and prosthetic joints, which may lead to bacteraemia or endocarditis and require the removal of the prosthesis. Biofilm production contributes to their pathogenicity.
Laboratory diagnosis
Staphylococcus epidermidis grows readily on laboratory media; coagulase is not produced. Speciation is by biochemical testing. DNA restriction patterns or other molecular techniques may be needed to determine whether strains are identical. S. epidermidis and other CoNS are common contaminants in blood cultures, requiring careful evaluation of their clinical significance.
Antibiotic susceptibility
This group of organisms is uniformly susceptible to vancomycin and usually to teicoplanin. They may also be susceptible to any of the other agents used for S. aureus infection, but this is unpredictable. Treatment must be guided by in vitro testing.
Less common than S. epidermidis, Staphylococcus haemolyticus causes a similar disease pattern. It differs from S. epidermidis in that it causes haemolysis on blood agar. More importantly, it is naturally resistant to teicoplanin; significant infections require vancomycin therapy.
Staphylococcus saprophyticus
These CoNS are a common cause of urinary tract infection in young women. They can be rapidly distinguished from other species by their resistance to novobiocin.