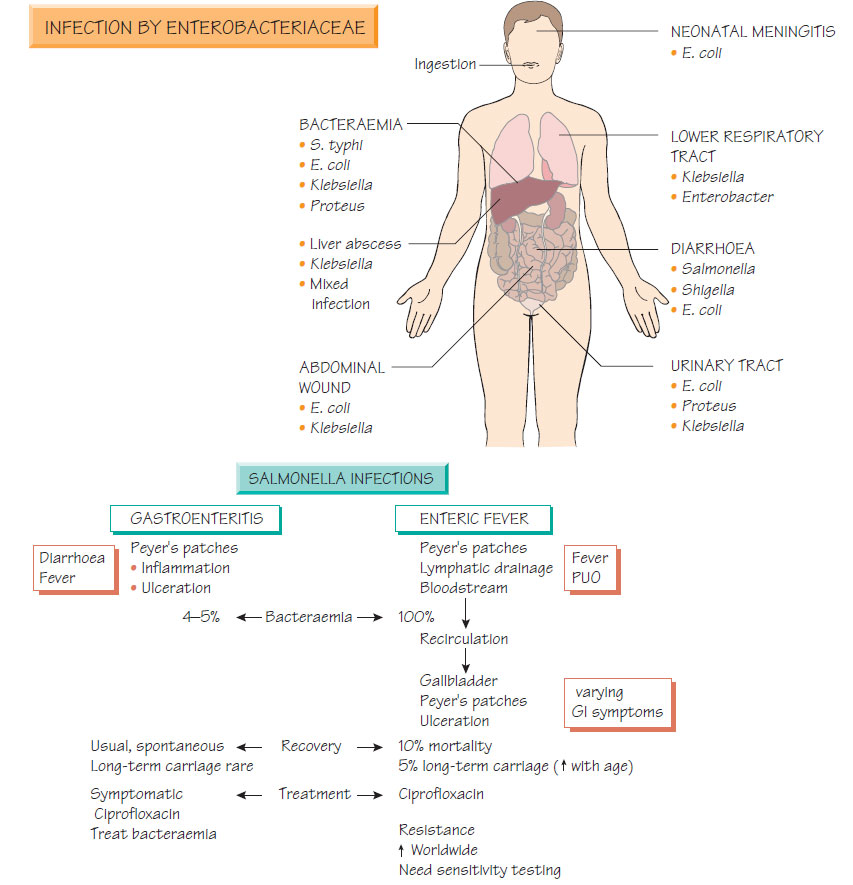
Enterobacteriaceae clinical syndromes
SalmonellaThere are two Salmonella species that account for the majority of human and animal infections: S. enterica and S. bongori.
Salmonellosis
Salmonella are host-adapted to animals and humans. Infection is usually confined to the bowel, appearing as acute self-limiting diarrhoea. Less commonly invasive disease develops, which may be complicated by bacteraemia, life-threatening septicaemia or osteomyelitis. Important sources of infection include domestic animals and the food produced from them, and human cases including convalescent carriers. Transmission is by the oral route, usually through ingestion of contaminated foods. Infection is commoner and often more severe in patients with reduced gastric acid and those who are immunocompromised or splenectomized. Reactive arthritis or a chronic carrier state may be complications of infection.
Enteric fever (typhoid) is caused by S. enterica serotype Typhi or Paratyphi. Invasion of the intestinal wall, with spread to local lymph nodes, is followed by primary bacteraemia and infection of the reticuloendothelial system. The bacteria reinvade the bloodstream and gut from the gallbladder, multiply in Peyer's patches, and cause ulceration that may be complicated by haemorrhage or perforation. Patients present with fever, alteration of bowel habit (diarrhoea or constipation) and, more rarely, the classical rash (rose spots on the abdomen). Hepatosplenomegaly may also be demonstrated. Enteric fever may be complicated by osteomyelitis and, rarely, by meningitis.
Other infections
Urinary tract infection and pyelonephritis
Most Escherichia coli urinary tract infections are caused by a limited number of serotypes related to specialized adaptations (e.g. presence of the K antigen, adherence to uroepithelial cells via pili and haemolysin production). Mannose-resistant pili are associated with pyelonephritis. Proteus spp. also possess specialized adherence pili that mediate attachment to urinary epithelium. Urease production by Proteus is the most important virulence determinant in urinary infection, lowering pH and precipitating stone formation.
Escherichia coli is an important cause of neonatal meningitis associated with a high mortality. Strains often express copious amounts of K1 capsular antigen. Meningitis may also follow neurosurgical procedures, especially when prosthetic devices are inserted. Enterobacteriaceae are often found as part of the polymicrobial flora of brain abscess.
Osteomyelitis and septic arthritis
Salmonella osteomyelitis or septic arthritis is an important complication for patients with sickle cell disease or AIDS and for older patients. Infection with other Enterobacteriaceae can also follow penetrating trauma when contaminated fragments are taken into the bony tissue. Treatment often includes a fluoroquinolone such as ciprofloxacin that penetrates into bony tissue.
Infection with Klebsiella spp. is usually acquired in a hospital environment. These organisms are an important cause of ventilator- associated pneumonia, urinary tract infection, wound infection and bacteraemia. Outbreaks of infection in high-dependency patients have been described and are associated with septicaemia and a high mortality. Primary pneumonia with K. pneumoniae subspecies pneumoniae is a rare, severe, community-acquired infection, associated with a poor outcome. K. rhinoscleromatis causes a progressive granulomatous infection of the nasal passages and surrounding mucous membranes. Most infections are found in the tropics. K. ozanae has been associated with chronic bronchiectasis. Enterobacter, Serratia and Citrobacter infections These are environmental organisms that may colonize and infect hospitalized patients, causing wound infections, bacteraemia and hospital-acquired pneumonia. Many isolates may be naturally resistant to antibiotics and treatment choices are limited.
Diagnosis
The Enterobacteriaciae grow readily on laboratory media and are identified by biochemical reactions, such as the pattern of fermentation of different sugars. Epidemiological investigation uses serotyping (sera directed against the lipopolysaccharide [O] antigens and flagellar [H] antigens), but molecular typing methods are gaining a place (e.g. sequencing of flagellar genes). In the case of typhoid, a diagnosis may be made by isolating organisms from the blood or bone marrow.
Most enteric Gram-negative organisms are susceptible to aminoglycosides, extended-spectrum cephalosporins, fluoroquinolones, β- lactams and carbapenems (e.g. meropenem). As some produce β-lactamases and aminoglycoside-degrading enzymes, treatment should be guided by sensitivity tests. Emerging extended-spectrum β-lactamase-carrying strains (ESBLs) increase the resistance to broad-spectrum antibiotics.
In urinary tract infections, cefalexin, ampicillin, nitrofurantoin or trimethoprim are the first-choice antibiotics. Diarrhoeal disease can be avoided by good hygiene, food preparation and safe water supplies. Treatment is primarily by oral rehydration (see Bacterial diarrhoeal disease).