Identification of Pneumococci
Pneumococci are among the most important agents of bacterial pneumonia. Other microorganisms such as staphylococci, Haemophilus influenzae (Experiment 22.1), and Klebsiella pneumoniae may also be associated with serious pulmonary disease. Bacterial agents of pneumonia cause an acute inflammation of the bronchial and/or alveolar membranes. When the alveoli are involved, their thin membranes may be disrupted by hemorrhage of alveolar capillaries and collections of inflammatory exudate (pus) containing many white blood cells. Laboratory diagnosis is often made by isolating the causative agent from sputum sent for culture. However, because sputum specimens pass through the oropharynx as they are expectorated, contaminating members of the normal throat flora may interfere with culture results by overgrowing the pathogen. The causative organism is often found in the bloodstream during early stages of infection, and therefore, patient blood should also be cultured. In some patients, the organisms spread from the bloodstream to the central nervous system to cause meningitis. Pneumococci can then be isolated from the patient’s cerebrospinal fluid as well.Pneumococci are classified in the genus Streptococcus as the species pneumoniae. They are gram-positive, lancet-shaped cocci that characteristically appear in pairs (diplococci) or in short chains (see colorplate 3). Like other streptococci, they are fastidious microorganisms and require blood-enriched media and microaerophilic conditions for primary isolation. They are alphahemolytic and usually produce greening of blood agar around their colonies. Streptococcus pneumoniae can be distinguished from other alpha-hemolytic streptococci because it is lysed by bile salts and other surface active substances, including one known as optochin (see colorplate 31).
Another distinctive feature of pneumococci is that they possess a capsule, composed of a viscous polysaccharide. This slimy capsule protects them from destruction by phagocytes that gather at sites of infection throughout the body to ingest them. In the laboratory, the pneumococcal capsules are not readily demonstrated by usual staining techniques, but they can be made visible under the microscope by a serological technique known as the “quellung” reaction. Quellung is the German word for “swelling” and describes the microscopic appearance of pneumococcal or other bacterial capsules after their polysaccharide antigen has combined with a specific antibody present in a test serum from an immunized animal. As a result of this combination, and precipitation of the large, complex molecule formed, the capsule appears to swell, because of increased surface tension, and its outlines become clearly demarcated (see colorplate 10).
The capsular antigen can also be detected with antibody-coated latex reagents. Colonies of suspected pneumococci growing on blood agar plates may be tested, or, depending on the disease severity, the soluble capsular antigen may be present in the patient’s CSF, blood, and urine (the antigen, but not necessarily the organisms, is excreted from the body by the kidneys). Regardless of the results of direct antigen detection tests, cultures of sputum, blood, and cerebrospinal fluid (in patients with signs and symptoms of meningitis) should always be performed. In some instances, the antigen concentration in body fluids is too low to be detected, but cultures are positive.
Pneumococci are frequently found among the normal flora of the upper respiratory tract of healthy individuals. Their recovery in sputum cultures is not, of itself, conclusive evidence of pneumococcal disease. This finding must be correlated with the total picture of the patient’s clinical illness.
| Purpose | To identify pneumococci in culture |
| Materials | Dropping bottle containing 10% sodium desoxycholate or sodium taurocholate (bile solution) Tubes containing 1 ml nutrient broth Optochin disks Forceps Blood agar plate Candle jar Blood agar plate cultures of pneumococci and other alpha-hemolytic streptococci |
Procedures
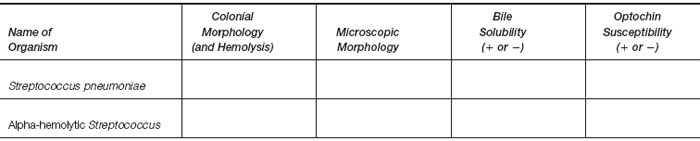
- Examine the blood agar plate cultures of pneumococci and of alpha-hemolytic streptococci and note any differences in colonial morphology. Make a Gram stain of each organism.
- Make a light but visibly turbid suspension of pneumococci in each of two tubes of nutrient broth. Repeat, making two suspensions of the other alpha-hemolytic streptococci in nutrient broth.
- To one tube of each suspended organism add a few drops of the 10% bile solution. Over a 15-minute period, observe all tubes for evidence of clearing of the suspension (lysis of the organisms) and record results for each tube.
- Mark a blood agar plate with your marking pencil to divide it in half. Streak one side heavily with a loopful of pneumococci, the other side equally with alpha-hemolytic streptococci.
- Flame or heat your forceps lightly and use them to take up an optochin disk. Place the disk in the center of the area on the
blood plate you streaked with pneumococci. Reheat the forceps and place another disk in the middle of the section
streaked with alpha-hemolytic streptococci. Press each disk down lightly on the agar with the tip of the forceps, to make
certain it is in contact and will not fall off when the plate is inverted (do not press it through the agar). Reheat the forceps.
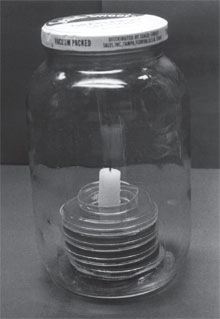
Note: Optochin is the commercial name for ethylhydrocupreine hydrochloride, a surface reactant impregnated in the disk. Its effect on pneumococcal cell surfaces is similar to that of bile. The disk is often called a “P-disk” because it is used to distinguish susceptible pneumococci from other streptococci that are not lysed by surface reactants. - Invert the plate and place it in a candle jar. Light the candle, replace the lid of the jar (tightly), and wait for the candle flame to burn out. Place the jar in the 35°C incubator for 24 hours. (Any wide-mouthed, screw-cap jar can serve as a candle jar. The candle burning in the closed jar uses up some of the oxygen and increases the carbon dioxide level. At a certain point, the oxygen is not sufficient for the candle to continue burning, and the flame will be extinguished. The atmosphere remaining within the jar contains the increased carbon dioxide tension and the reduced oxygen tension preferred by many bacterial species, such as pneumococci, when they are first removed from the body and cultured on artificial medium (fig. 21.3.) In many clinical laboratories, the plates are incubated in a special CO2 incubator. Gas flowing into the incubator from a CO2 cylinder maintains a constant level of 5 to 7% CO2.
Results
|
|
 |