Ocular infections
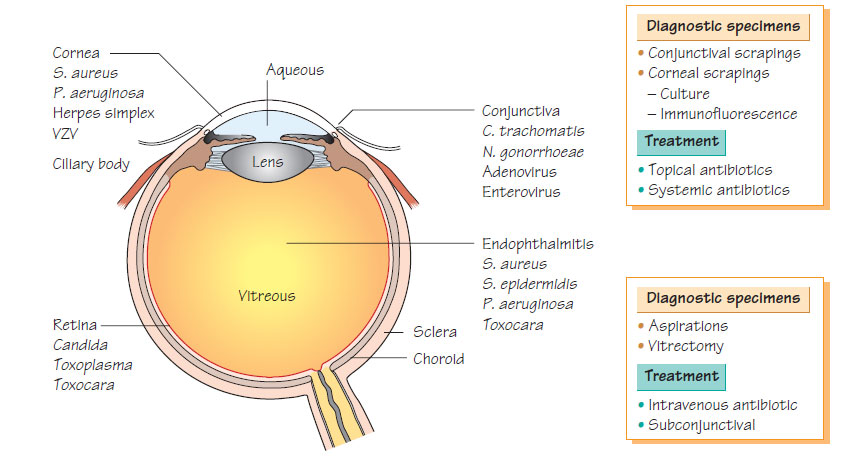
Bacterial conjunctivitisBacterial conjunctivitis is common and caused by Staphylococcus aureus, Haemophilus influenzae, Streptococcus pneumoniae or Moraxella spp. Neonatal conjunctivitis is acquired from infection in the mother's genital tract and caused by Neisseria gonorrhoeae, Chlamydia trachomatis, Escherichia coli, S. aureus and H. influenzae. In hospital if ocular equipment or drops are not adequately sterilized or restricted to a single use, infection with Pseudomonas aeruginosa may occur. Infection is also associated with contaminated personal contact-lens cleaning equipment. Pseudomonas infection may be rapidly progressive, resulting in ocular perforation and loss of vision. Bacterial conjunctivitis presents with hyperaemic, red conjunctivae and a profuse, mucopurulent discharge. Conjunctival swabs and corneal scrapings are submitted for laboratory examination. The diagnosis is confirmed by bacterial culture or nucleic acid amplification test (NAAT) including for C. trachomatis. Treatment is with local antibiotics, which include fusidic acid, tetracycline chloramphenicol or fluoroquinolones.
Half of the adenovirus serotypes have been associated with ocular infection, but types 7, 3, 11, 19 and 37are most commonly associated.
- Purulent conjunctivitis occurs, with enlargement of the ipsilateral periauricular lymph node.
- Corneal involvement leads to punctate keratitis and subepithelial inflammatory infiltration, anterior uveitis and conjunctival haemorrhages.
- Treatment is symptomatic, with antibacterial agents being used if there is evidence of secondary bacterial infection. Topical steroids should be avoided. New drugs are in early phase trials.
Varicella zoster virus
The ophthalmic dermatome of the fifth cranial nerve is involved in approximately 10% of recurrent varicella zoster virus (VZV) infections (shingles). Ocular involvement, manifests in anterior uveitis, keratitis, ocular perforation or retinal involvement. Chronic disease occurs in about one-quarter of patients. The condition is very painful and pain may continue after healing of the rash (Postherpetic neuralgia). Antiviral agents (e.g. aciclovir) should be used early in the infection and may prevent complications. Severe inflammation may benefit from topical steroids. A live attenuated vaccine is available to prevent primary infection.
Ocular infection with herpes simplex is the most common infectious cause of blindness in developed countries.
- Ulcerative blepharitis, corneal involvement, follicular conjunctivitis and regional lymphadenopathy occur.
- Relapses occur approximately every 4 years.
- Initially, a dendritic ulcer is present, but the later clinical picture is dominated by inflammation in deeper tissues, keratitis, corneal oedema and opacity.
- Primary infection and early relapses are treated with topical aciclovir. Steroids worsen the keratitis.
- Progressive scarring that follows repeated attacks leads to corneal opacity and is a common indication for corneal grafting.
Ocular manifestations of AIDS
'Cotton wool spots' are a common retinal manifestation of untreated HIV infection due to infarction of the retinal nerve fibre layer. Cytomegalovirus (CMV) and fungal infection may develop in patients with very low CD4 counts. CMV causes a slowly progressive retinitis characterized by necrosis and may lead to blindness. The syndrome is difficult to differentiate from ocular toxoplasmosis or syphilitic retinitis. Initial treatment with parenteral ganciclovir followed by weekly maintenance therapy to prevent relapse is used. Immune-recovery uveitis can occur after the introduction of highly active antiretroviral therapy (HAART).
- Trachoma is a chronic keratoconjunctivitis caused by infection with C. trachomatis, which is now largely confined to the tropics, where poor social conditions make transmission easier and poverty reduces access to health care.
- Symptoms develop 3-10 days after infection, with lacrimation, mucopurulent discharge, conjunctival infection and follicular hypertrophy. Treatment is with oral macrolides, such as azithromycin.
- An international campaign plan to eradicate trachoma by 2020 is under way using the SAFE strategy (Surgery for in-turned lids, Antibiotics, Face washing and Environmental improvement).
- Endophthalmitis can develop after an ocular operation, following trauma, due to the presence of a foreign body or as a complication of systemic infection.
- Early postoperative infections are commonly with S. aureus, Staphylococcus epidermidis, streptococci or Gram-negative bacilli.
- Late postoperative infections are with streptococci or H. influenzae.
- Post-traumatic infections are caused by S. epidermidis, Bacillus and streptococci.
- Endogenous infections secondary to bacteraemia or fungaemia are most often with Candida, streptococci and enteric Gramnegative bacilli.
- Rarely, endophthalmitis is caused by the nematode Toxocara canis (see Zoonoses).
- The diagnosis is made by vitreous aspiration or vitrectomy specimens.
- Bacterial endophthalmitis is managed by systemic antibiotics or intravitreal injection, depending on the spectrum and pharmacokinetics of the agents.