Hepatitis viruses
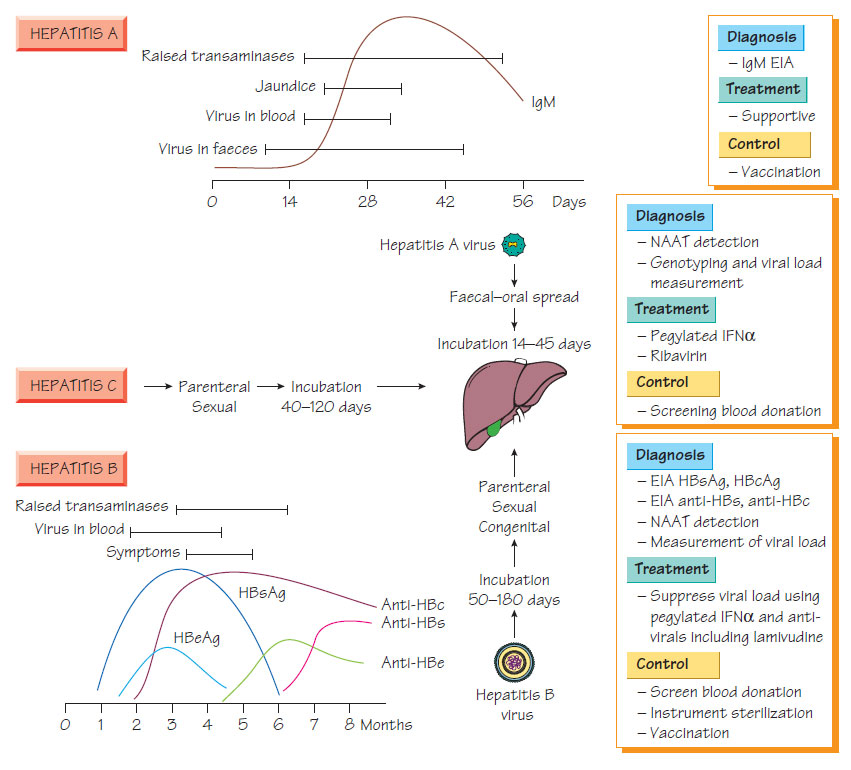
Hepatitis AHepatitis A virus (HAV) is a Hepatovirus related to the Enteroviruses (see Enterovirus and viruses that infect the gastrointestinal tract) with four genotypes. Transmission is by the faecal-oral route. Institutional outbreaks are associated with summer and point-source outbreaks follow faecal contamination of water or food (e.g. oysters). Seroprevalence is highest in individuals of lower socioeconomic groups. Anicteric infection is more common in the young; the risk of symptomatic disease increasing with age. Infection is characterized by a 'flu-like illness followed by jaundice, with most patients making an uneventful recovery. Virus is shed in stool before jaundice appears.
Diagnosis
- Anti-HAV IgM is diagnostic appearing before jaundice develops and persisting for 3 months.
- IgG antibodies determine a patient's immune status.
- HAV RNA can be detected in the blood and stool during the acute phase of infection by nucleic acid amplification test (NAAT).
Treatment is symptomatic and chronic hepatitis does not occur. Adequate sanitation and good personal hygiene will reduce the transmission of HAV. Vaccination against HAV is recommended for travellers to high-risk areas, patients with chronic liver infection and individuals with high-risk occupations (e.g. healthcare workers, sewage workers). Passive immunity can be provided using human immunoglobulin. http://www.dailymotion.com/video/xto5x9 Hepatitis B (HBV), a hepadnavirus, is an enveloped virus that contains partially double-stranded DNA encoding surface antigen (HBsAg), core antigen (HBcAg), pre-core protein (HBeAg), a large active polymerase protein and transactivator protein. The virus replicates through a reverse transcriptase. HBV is transmitted by parenteral, congenital and sexual routes. A quarter of the global population is infected.
- HBV infection has a long incubation period (up to 6 months).
- Acute hepatitis of variable severity develops insidiously.
- Fulminant disease carries a 1-2% mortality and 10% of patients develop chronic hepatitis complicated by cirrhosis or hepatocellular carcinoma.
- Congenital infection carries a high risk of hepatocellular carcinoma.
Diagnosis
- Immunoassays for HBsAg, HBeAg, HBcAg and associated antibodies enable the diagnosis of acute infection and previous exposure (see Figure).
- Viral load can be measured by NAAT and sequencing for resistance mutations allows monitoring of therapy and directs drug choice.
- Pegylated α-interferon.
- Lamivudine, adefovir, entecavir, tenofovir, telbivudine and clevudine have antiviral efficacy. Emtricitabine and valtorcitabine are nearing clinical introduction.
- Therapy should be considered in chronic infection as responders have a reduced risk of liver damage and liver cancer in the longterm. HBeAg seroconversion is often taken as a mark of Treatment success.
- Those at high risk should be immunized with recombinant HBV vaccine.
- Vaccine and specific immunoglobulin should be administered to neonates of infected mothers to reduce transmission.
- Blood donations must be effectively screened.
- Needle-exchange programmes for drug misusers and sexualhealth education schemes can help to reduce transmission.
Hepatitis C (HCV) is a sense RNA virus encoding a single polypeptide. Transmission is mainly through infected blood. Seroprevalence is approximately 1% in healthy blood donors, higher in developing countries and highest in high-risk groups, such as those who have received unscreened transfusions. Healthcare workers are at risk. Sexual transmission and vertical transmission do occur but are uncommon.
Clinical features
Infection may cause a mild acute hepatitis but many cases are asymptomatic; fulminant disease is rare. HCV infection persists in up to 80% of patients; up to 35% of these develop cirrhosis, liver failure and hepatocellular carcinoma between 10 and 30 years later. This occurs because frequent virus mutation results in immunologically distinct 'quasi-species', which allow the organism to escape immunological control.
Diagnosis
- HCV cannot be cultured.
- Diagnosis is by antibody and antigen detection.
- A NAAT is available.
- Sequencing to determine genotype defines the likelihood of response to therapy (see below).
- Treatment is monitored by measurement of viral load.
- Ribavirin and pegylated α-interferon.
- Response is best in patients with genotypes 1 and 2 and those with low initial viral load, but up to 80% will clear the virus.
- Liver fibrosis or necrotic inflammation from HCV infection is an indication for liver transplantation.
- Preventive measures are similar to those employed against HBV.
- There is no vaccine.
Hepatitis D
This defective RNA virus is surrounded by an HBsAg envelope and is transmitted with and in the same way as hepatitis B virus or as a super-infection in an HBV carrier. Although asymptomatic infection may occur, hepatitis D (HDV) is associated with severe hepatitis and an accelerated progression to carcinoma. A real-time NAAT is the most rapid method of making the diagnosis but antigen detection or IgM antibody detection by enzyme immunoassay (EIA) can also provide confirmation. Preventive measures for HBV also protect against HDV.
- Hepatitis E is a small, single-strand, non-enveloped RNA virus.
- Transmission is by the faecal-oral route.
- Outbreaks occur after contamination of water supplies or food.
- It is found in Asia, Africa and Central America.
- It usually causes a self-limiting hepatitis of varying severity.
- Diagnosis is by IgM or NAAT.
- Infection is prevented by hygiene measures.
Viral hepatitis can also be caused by other viruses (e.g. cytomegalovirus [CMV], herpes simplex and Epstein-Barr virus [EBV]).