Emerging infections
The incidence of an infection varies with changes in pathogen virulence and in the immunity of the host population. Many infectious diseases have a characteristic pattern. For example, meningococcal infection in the 'meningitis belt' of Africa is endemic (cases occur all of the time), but the incidence of the disease will sometimes rise to 1000 per 100 000 of the population - an epidemic.The words 'outbreak' and 'epidemic' are often used interchangeably, although an outbreak can be thought of as a localized epidemic. Pandemics occur when an epidemic spreads worldwide. Examples of pandemic diseases include influenza after the organism undergoes an antigenic shift (see Influenza viruses), plague (Small Gram-negative coccobacilli: Haemophilus, Brucella, Francisella, Yersinia and Bartonella) and cholera (Vibrio, Campylobacter and Helicobacter).
New or emerging infections are important because 'new' diseases may not be recognized immediately, so may remain undiagnosed. Emerging diseases fall into three broad categories:
- new pathogens;
- established pathogens invading new territories;
- re-emergence of a previously controlled organism.
New pathogens
Several of the most important emerging infections have arisen because they are genuinely new infections. The most important example of this is the human immunodeficiency virus (HIV), which is thought to have emerged from simian immunodeficiency virus (SIV) by jumping species from chimpanzees to humans in central Africa over 50 years ago (see HIV infection and AIDS). Severe acute respiratory syndrome (SARS) was caused by a novel coronavirus that jumped into humans in southern China; fortunately this infection was controlled rapidly. Invasion of forest habitats has brought humans into contact with Trypanosoma cruzi, which lead to infections.
Climatic change or changes in population centres may permit an organism to invade new territory. For example, infection with West Nile virus is spreading in the USA at present, entering some states for the first time. Climate change may allow vectors to change their range and permit diseases like malaria to invade/reinvade new territories.
Re-emergence of previously uncommon infections
Effective treatment and organized control programmes had been reducing tuberculosis; however, migration and synergy with HIV has now increased the number of cases globally. Loss of confidence in MMR resulted in a reduction in vaccine uptake, which resulted in localized outbreaks of measles that showed that many infectious diseases await their opportunity to re-emerge. The development of multiple-drug resistance may allow other organisms to re-emerge (e.g. multidrug-resistant tuberculosis [MDRTB]).
The spread of organisms in livestock herds or flocks, such as strains of Salmonella enteritidis, may provide new opportunities for contamination of products in the food chain. The widespread use of pre-prepared chilled food has increased the risk of listeriosis.
Changes in the virulence or transmissibility of a pathogen
Some pathogens may emerge in particular niches because they are more virulent or more easily transmitted. Clostridium difficile 027 has caused hospital outbreaks in Canada, the USA and the UK. Multiple drug-resistant Acinetobacter baumanni has caused outbreaks in intensive care units. Epidemic MRSA EMRSA-15 and ERMSA-16 have caused outbreaks in many settings and are now the predominant strains of MRSA worldwide.
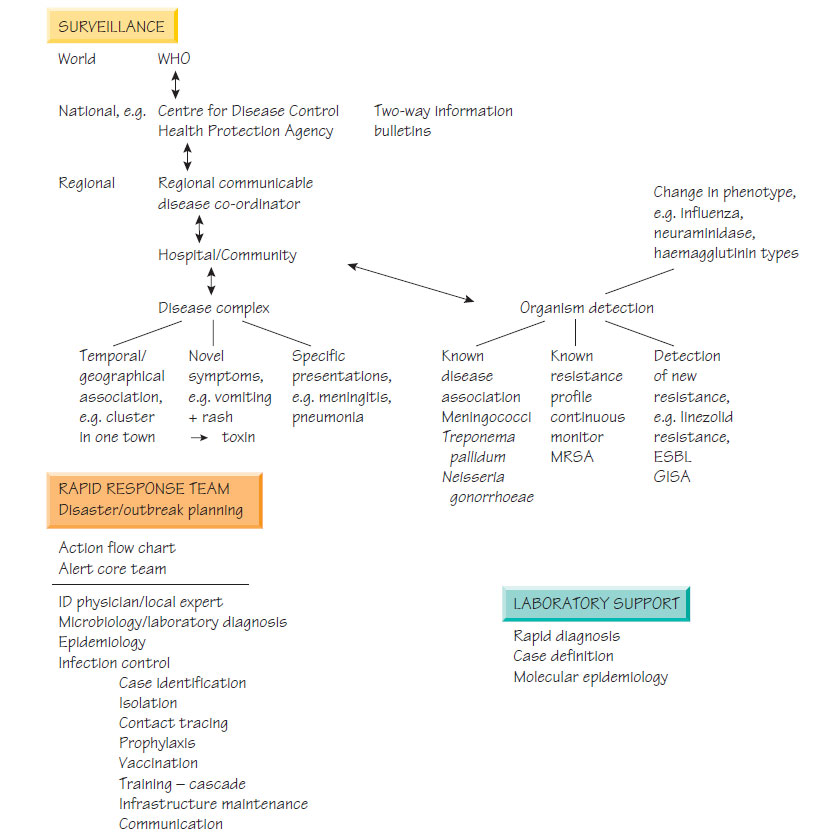
Political uncertainty and terrorist activity raise the risk that microbes could be used as biological weapons. One bioterrorism incident using anthrax occurred in the USA and resulted in four deaths and the need to create extensive control measures. Other agents of concern include smallpox, tularaemia, plague and a number of viral haemorrhagic fever viruses. Healthcare professionals need to know about the signs of these unusual infections and how to communicate concerns to the relevant agencies so that changing patterns can be identified quickly and interventions rapidly deployed (see Principles of infection control).